Let’s explore the important role accounts payable plays in the success of your business and how you can optimize your accounts payable systems and processes healthcare accounts payable for greater efficiency. Health systems that proactively negotiate terms, leverage group purchasing organizations, or secure extended payment windows can reduce the cost of goods sold while improving overall liquidity. They recognize the time constraints of our staff and require minimal effort on our part to conduct the review. The claim documentation supplied to our vendors is accurate, well-supported and easy to understand. Handles Billing and Collections Some providers offer full healthcare receivables management, reducing administrative work and helping improve collection rates. After validation, the invoice enters the approval workflow, which is pre-defined based on the organization’s policies and procedures.
- Route approvals intelligently, PO match efficiently, and schedule batch payments accurately, every time.
- Seamless integration with your ERP, centralized vendor management, and detailed audit trails protect both financial and patient data.
- For hospitals where every dollar saved supports patient care, these gaps matter.
- With thousands of vendors and a constant flow of transactions, even small inefficiencies in Accounts Payable can create meaningful financial leakage.
- Partnering with a professional medical billing and RCM company, like MediBillMD can save you the stress.
What Does Payment Deferred Mean and How Does It Work for Businesses?
There are also reams of paper to manage, which compounds if each of their healthcare partners engages in manual processes. Moreover, each hospital or health system has its own way of doing things, and the supplier must respond to those various needs, adding to the complexities and resource intensiveness of managing incoming payments. Finally, a paper process does not give the supplier any insight into its performance against agreed payment terms or allow it to identify opportunities for better financial results. APS stays on top of the latest trends and best practices in healthcare accounting.
Invoice Approval Workflow
Accounts payable is the opposite side of the financial equation and represents the organization’s liabilities. The RCM industry experts recommend healthcare organizations maintain their average days in accounts receivables to 35 days or less to ensure a steady cash flow and healthier revenue cycle. Unlike other industries, there are a lot of spokes in the wheel for healthcare.
Find out more about MHC’s solutions for the Healthcare industry!
In a healthcare organization, the accounts payable department is typically responsible for handling all aspects of the organization’s accounts payable process. This includes issuing and tracking invoices, processing and paying vendor bills, reconciling vendor statements, and maintaining accurate records of all accounts payable transactions. The accounts payable department may also be responsible for working with the organization’s finance team to manage cash flow and ensure that all payments are made in a timely and accurate manner. Depending on the size and structure of the healthcare organization, the accounts payable department may be a standalone unit or it may be part of the finance or accounting department. Accounts receivable represent the money owed to providers for medical services delivered but not yet paid for.
It helps healthcare organizations avoid unnecessary borrowing, reduce financial stress, and maintain good relationships with vendors and suppliers. By ensuring payments are received and disbursed on schedule, providers can plan confidently, invest in improvements, and continue delivering high-quality patient care without disruption. By providing real-time visibility into payments, hospitals and clinics can more effectively manage their cash flow. AP systems also allow healthcare providers to easily track receivables and payables, enabling them to stay on top of their financial obligations.

The Cure for Overspending: Cashback Cards for Medical Clinics
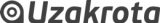
The healthcare industry is constantly faced with new dilemmas, ever-shifting priorities, and increased volume when it comes to its Accounts Payable process. Automate your AP operation with cloud-based MHC NorthStar and reduce manual intervention, data discrepancies, and security and compliance concerns. Finally, evaluating user reviews income statement can provide a more personal perspective on how different systems perform in real-world settings. The fifth section should focus on common challenges when implementing an AP system in a hospital or clinic. This includes data entry errors, data security, integrating the system with existing systems, user acceptance, and ongoing maintenance. Data entry errors can occur if staff do not enter data correctly or if data is not entered in a timely manner.
MHC NorthStar gives you the ability to configure and modify workflows as needed, including allowing the AP Manager to approve the invoice when certain stakeholders are unavailable. Stakeholders receive notification that an invoice is ready for approval and can submit for final payment at the click of a button. PubMatic streamlined global mass payments, cut processing time to 3 minutes, and enhanced operations with a robust NetSuite ERP integration. Tipalti’s customer, Acuity Eye Group, has been using Tipalti AP automation software integrated with NetSuite ERP since 2018. Acuity Eye Group reduced its 80% payables workload across 12 subsidiaries and 50 Bookkeeping 101 locations by implementing Tipalti AP automation with multi-entity capabilities. The cost of an AP system should also be taken into account when selecting one.
Avoiding Timesheet Errors: A Practical Guide for Project-Based Teams
However, it could save up to $25 billion (41%) by completely automating the administrative transactions. One of the many challenges you may encounter is the failure to track and streamline your A/R processes. The second step is to collect all the necessary information for invoicing, like details about the care services, their medical necessity, patient’s details, etc. Missing or incorrect information is another main reason leading to medical claim denials.